2016-2017 Research Report
MAJOR RESEARCH ADVANCES FROM OUR DEPRESSION TASK FORCE IN 2016-2017
The researchers of HDRF’s Depression Task Force came together five years ago with one overarching strategy: To identify the genes, molecules and circuits that cause depression, and to use that knowledge to drive new treatments.
The value of their work cannot be overstated. Finding new treatment options is crucial, since 50% of patients do not respond to available anti-depressants.
The Depression Task Force has made clear and steady progress in this endeavor. In September of 2017, the team of seven world-acclaimed brain scientists published a major review: Treatment Resistant Depression: A Multi-scale, Systems Biology Approach in the prestigious journal Neuroscience and Biobehavioral Reviews.
Here are the highlights
- In the past year, the Task Force has discovered several novel approaches to new treatments, and three new compounds are now in clinical trials.
- They have identified specific patterns of neurons in the brain that become over-active or under-active in depression.
- They have started to map the genetic architecture of these regions, to identify key genes and gene clusters that may be at the root of depression.
These discoveries would not have been possible without the unique collaboration of Depression Task Force. Their ability to pool expertise and data across multiple universities is a model for the entire field.
PUBLICATIONS
In 2016-2017 the Depression Task Force published their findings in over 40 articles in major publications such as:
- American Journal of Psychiatry
- Nature
- Biological Psychiatry
- JAMA Psychiatry
- Molecular Psychiatry



NEW DRUGS NOW IN CLINICAL TRIALS AS A RESULT OF HDRF-FUNDED RESEARCH
- L Acetyl Carnitine:
L-Acetyl Carnitine (LAC) is an amino acid that is naturally produced by the body. Work in the lab of DTF member Dr. Bruce McEwen’s has shown that LAC levels in the brain are a key determinant of depression risk in laboratory mice. Clinical trials are now underway at Rockefeller University to test LAC on a sample of treatment resistant individuals. It is believed that LAC improves cell efficiency and helps to increase the number of receptors in the brain that regulate stress. - Tianeptine
Currently the Depression Task Force is planning a small clinical trial of the atypical antidepressant Tianeptine. This drug has been used clinically in Europe for 30 years, but its direct molecular target has been unclear. Work by DTF members Drs. Rene Hen and Jonathan Javitch has proven that Tianeptine binds selectively to a specific type of opioid receptor – a receptor system that regulates pain. This receptor has never before been believed to be important for depression. Tianeptine has emerged therefore as a very exciting candidate for developing new therapeutics. The DTF pilot study will target a subset of depressed patients with high levels of rejection sensitivity, based on the belief that the opioid receptor system is key in mediating rejection sensitivity. - Ezogabine
Recently Mount Sinai conducted a pilot clinical study of Ezogabine on 20 individuals with treatment resistant depression. Ezogabine is an existing FDA-approved treatment for mild epilepsy. The idea for using Ezogabine came from work by DTF member Dr. Eric Nestler which showed that elevated electrical activity in a key brain circuit can cause depression in laboratory mice. Ezogabine is known to target this micro-circuit. The resulting data showed a significant improvement in depressive symptoms in humans.
These pilot data have now led to a successful NIMH grant to start Clinical Phase 2 Trials, a key step to bringing a new drug to the millions who need it.
MEMBERS OF THE HDRF DEPRESSION TASK FORCE, 2017

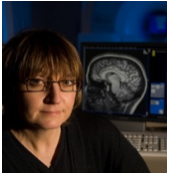
Huda Akil, PhD, University of Michigan, DTF Chair
Molecular and Behavioral Neuroscientist, Neurogeneticist
Expertise: Lead researcher of genes and proteins that cause vulnerability to major depression; expert in the brain biology of emotions, stress and depression.
Akil is addressing the fundamental question of why some people are susceptible to depression. She is looking for the genes that can make us vulnerable to depression and genes that can make us resilient to depression. She is sequencing the genomes of two laboratory rat lines she has selectively bred for resilient or vulnerable behavior. She is also comparing the anatomy and activity of their brain circuits.

Eric Nestler, MD, PhD, Mount Sinai School of Medicine
Molecular Psychiatrist, Neurobiologist
Expertise: Molecular neurobiology of addiction and depression; epigenetic regulation of DNA activity in brain.
Nestler is looking at how repeated bouts of stress throughout life produce lasting chemical changes in the brain circuits deemed to cause depression. Using advanced techniques, he is creating a “time-lapse” photo of the molecules in the brain that change during depression.

Michael Meaney, PhD, Douglas Institute & McGill University
Neurologist, Epigeneticist, Neurogeneticist
Expetise: Studies the effects of early adversity on gene expression and brain development; expert in epigenetics.
Experience and the environment may contribute to depression in a surprising way: by causing “epigenetic” changes – ones that turn genes on or off without altering the genes themselves. Dr. Meaney’s research shows how adversity early in life can permanently change the expression of key genes – and as a result increase the risk of developing depression later in life.

Bruce McEwen, PhD, Rockefeller University
Neuroendocrinologist, Leading Neuroscientist in Stress Research
Expertise: Investigates the effects of stress on brain centers involved in emotion, fear, memory and mood control; expert in the neuroscience of stress and emotion and its consequences for the body as well as the brain.
McEwen’s research has shown that chronic stress can alter the metabolism and fitness of circuits in the brain which regulate mood and emotion; certain circuits shrink, while others swell. He is now mapping the genetic architecture underlying these circuits to single out genes that change during depression.
Helen Mayberg, MD, Emory University
Neurologist, Leader in Neuro-imaging
Expertise: Examines neural systems mediating mood and emotions with a primary emphasis on major depression and its recovery; pioneer in Deep Brain Stimulation (DBS) as a therapeutic for treatment-resistant depression.
Dr. Mayberg is a pioneer in Deep Brain Stimulation to treat severe, resistant depression. In DBS, a pair of electrodes is implanted in a precise area of the brain and connected by wires to a pair of pulsing devices in the chest. The electrodes emit a kind of jamming signal to circuits in the brain known to be involved in depression, while leaving other circuits intact. Her work is helping the DTF refine our knowledge of the neural circuits that underlie depression.

Rene Hen, PhD, Columbia University
Neuropharmacologist, Neurogeneticist
Expertise: Investigates specific serotonin receptors as well as new nerve growth in the hippocampus in pathological states such as depression and anxiety; expert in neurogenetics.
Hen’s research focuses on the hippocampus — a brain area involved in learning, memory and emotion. He has discovered that new, “rookie” neurons generated in the hippocampus help us become resilient to depression. Interventions that can specifically boost the number of rookie nerve cells produced by the hippocampus may provide new ways to treat depression.

Jonathan Javitch, MD, PhD, Columbia University
Psychiatrist, Biochemist, Biophysicist
Expertise: Studies the detailed structure and function of proteins that are important for psychiatric phenomena.
Javitch’s research focuses on synapses — the spaces where signals pass between our brain cells. In particular he studies the transmitters that carry the signals and the receptors that “catch” the signals. He has discovered that a system of receptors involved in pain regulation may also be critical to the understanding of depression. These receptors were never before thought to play a role in depression, but Javitch has provided definitive proof that they do.
THE HDRF DATA CENTER, LOCATED AT THE UNIVERSITY OF MICHIGAN

Finding the Smoking Gun in the Data
Each of the HDRF projects is generating a huge amount of data. The HDRF Data Center is therefore critical for the mining of data from the various component labs to extract new knowledge about common changes that lead to depressive behavior. By converging data sets, the Depression Task Force have been able to identify a handful of brain molecules and genes that are prime candidates for study as new targets for depression treatment.